Study: 1.6 Million More Excess Deaths Among Blacks Compared To White People Since 2000
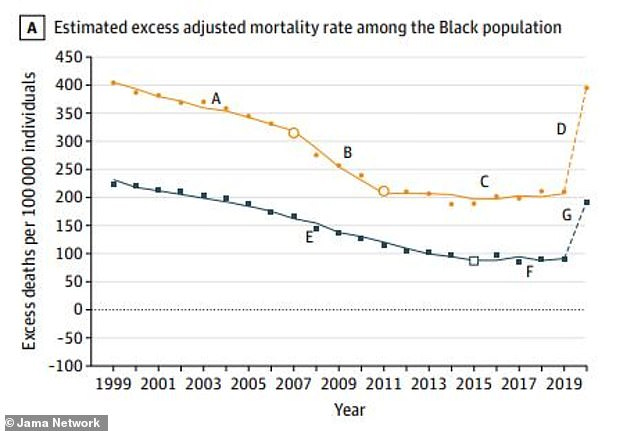
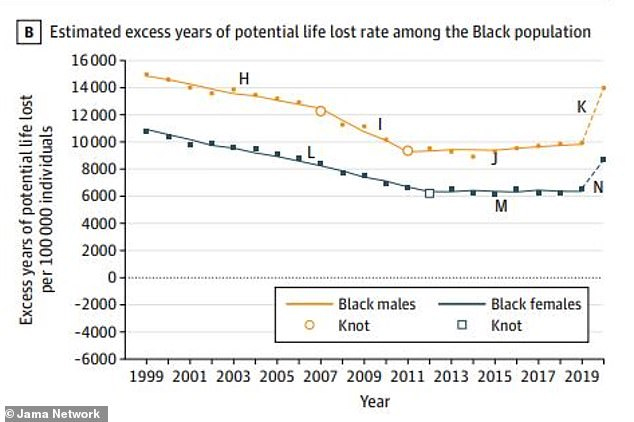
The disparity between white and Black mortality rates has been laid bare by a new study. Researchers from Yale and the University of Massachusetts found that Black Americans had 1.63 million excess deaths (the difference between the expected and actual number of deaths) relative to white Americans between 1999 and 2020.
The skyrocketing number of deaths during the Covid pandemic, particularly among Black Americans, saw two decades of progress closing the gap between Black and white mortality rates wiped out.
Structural racism, leading to police and gun violence and living in poorer areas, bigger barriers to health care as well as higher rates of heart disease, cancer, and infant and maternal mortality are to blame.
Historically, Black Americans are less likely to have access to healthcare which worsens their outcomes for every illness.
They are more likely to be living in poorer communities, which in turn means they are more likely to be exposed to drugs and alcohol and get caught up in gang violence.
Every day, roughly 26 Black Americans die from gun violence and they are 10 times more likely than white Americans to die from gun homicide.
In the US, Black adults are almost twice as likely to develop type 2 diabetes and also 30 percent more likely to die from heart disease than non-Hispanic white.
Black families having less money also leads to poorer diets and the consumption of less fruit and vegetables.
Black Americans also have less access to condoms which means a higher risk of STIs.
The country had made progress in reducing the Black mortality rate from 1999 to 2011, but that ground to a halt from 2011 to 2019.
The higher mortality rate between 1999 and 2020 meant a cumulative loss of more than 80 million years of life compared to white people.
The researchers said the study, published Tuesday (May 16) in JAMA, should be a ‘call to action’ to policymakers to address ‘structural racism, unmet social needs, and systemic bias’.
They used national US death certificate data from the Centers for Disease Control and Prevention as well as the annual life expectancy by five-year age groups from the National Center for Health Statistics to estimate the number of excess deaths.
The greater mortality rates among Black people are not so much to do with genetic factors but rather the long-time discrimination they have suffered, said Clyde Yancy, study author and chief of cardiology at Northwestern University.
Black neighborhoods that were deemed too ‘high risk’ for investments such as mortgages in the 1930s still have less money and higher illness rates, he said.
Formerly redlined ZIP codes also had more Covid infections and deaths.
Dr. Yancy said: “It’s very clear that we have an uneven distribution of health. We’re talking about the freedom to be healthy.”
Early deaths are due to higher rates of heart disease, cancer, and infant mortality.
Heart disease in both genders and cancer in males were the biggest drivers of differences in excess deaths, the study said.
When Covid hit, Black Americans were also dealing with ‘persistently higher barriers to health care, higher prevalence of multi-morbidity, and worse average health status’.
Herman Taylor, study author and director of the cardiovascular research institute at the Morehouse School of Medicine, said: “The study is hugely important for about 1.63 million reasons. Real lives are being lost. Real families are missing parents and grandparents. Babies and their mothers are dying. We have been screaming this message for decades.”
A similar study found that racial and ethnic inequalities cost the US more than $421 million in 2018 due to medical expenses, lost productivity, and premature death.
In 2021, the life expectancy of a non-Hispanic white American at birth was 76 years, while a non-Hispanic Black American was only 71.
This is partly because non-Hispanic Black children are 2.5 times more likely to not make it past their first birthdays, compared to white newborns.
And non-Hispanic Black mothers are more than three times more likely to die because of a pregnancy-related issue.
A pregnant woman in New York opened up about making the difficult decision to have a home birth amid the coronavirus pandemic because she feared ‘hospitals aren’t safe for Black women’ like herself.
Black women generally have the highest maternal mortality rates in the US.


