Is It A Ministroke? Know The Warning Signs Of A TIA
In her mind, she was talking — relaying to her hairstylist stories from her recent trip to Rome. But as Beth Bonness looked at herself in the mirror, dye still in her hair, she could see her mouth wasn’t moving. That’s weird, she thought.
Snowflake-like lights appeared on the side of her left eye, and her right hand curled into a claw. Her stylist — asking Bonness if she was OK; if she needed help — sounded like she was underwater.
“And there was pressure, but no pain,” says Bonness, of Portland, Oregon.
The whole thing lasted a few minutes — maybe four, she recalls. So Bonness, then 49, finished up her hair appointment, met her family for dinner at a nearby restaurant, then went home and filled her husband in on the strange events of the afternoon.
Soon after, Bonness was in the emergency room getting checked out. It was there she learned, her blood pressure was sky high, and she likely had a transient ischemic attack, or TIA, which happens when blood flow to the brain is temporarily blocked. Roughly 240,000 Americans a year have a TIA, sometimes called a ministroke, according to the American Stroke Association. And though they can occur at any age, they’re most common among adults 55 and older.
Bonness went home with blood pressure medication and a plan to take it easy for a few days.
It’s not uncommon for symptoms such as the ones Bonness experienced to be brushed aside, says Hardik P. Amin, M.D., associate professor of neurology and medical stroke director at Yale New Haven Hospital St. Raphael Campus in Connecticut. A big reason: When it comes to a TIA, there’s no pain involved.
“Usually if there’s a pain component, that’s going to send folks running to the hospital,” Amin says. “Here, it’s more like a loss of ability to do something.” And that loss of ability quickly resolves, often within a few minutes.
A short-lived weakness or numbness in the arm? “Sometimes patients just think, Oh, I just slept on it funny. I’ll try to shake it off or just kind of work through it and see if it just gets better on its own,” Amin says.
Bonness, who was a busy working mother, admits that when her TIA was happening, “there was a soft little part” of her that thought it could be stroke related. But with everything going on in her life, she says, “there wasn’t a lot of air space for the quiet warning signs to percolate.”
Doctors, however, say it’s important not to overlook TIA symptoms. In fact, they require immediate medical attention, a new scientific statement from the American Heart Association (AHA) says. Diagnosing a TIA and understanding its root cause can help prevent a full-blown stroke, which can cause lasting brain damage and long-term disability — even death.
“TIAs can be a harbinger of something really bad,” says Arif Jivan, M.D., an interventional cardiologist at Northwestern Medicine Lake Forest Hospital. “It can be a warning sign for a more significant stroke in the future.”
According to the AHA, up to 18 percent of people who experience a TIA will have a stroke within three months — and half of those strokes will occur within a few days. About one-third of people who have a TIA go on to have a stroke within a year.
Several days after her first TIA, Bonness found herself back in the emergency room. This time the diagnosis was a stroke.
What are the signs of a TIA?
The symptoms of a TIA are the same as those of a stroke, doctors say, only they are temporary and can sometimes resolve as quickly as they come on.
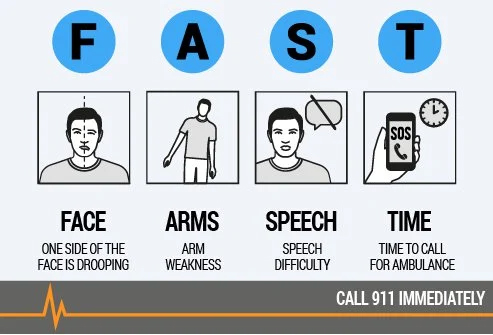 Amin points to the acronym FAST to recognize the warning signs of both TIA and stroke. The first three letters stand for: Face drooping (typically on one side), arm weakness or numbness (again, this is usually on one side of the body) and speech difficulty, where an individual may struggle to string words together, may say something nonsensical or may have thick, slurred speech “where it sounds like the patient’s got marbles in their mouth,” Amin says.
Amin points to the acronym FAST to recognize the warning signs of both TIA and stroke. The first three letters stand for: Face drooping (typically on one side), arm weakness or numbness (again, this is usually on one side of the body) and speech difficulty, where an individual may struggle to string words together, may say something nonsensical or may have thick, slurred speech “where it sounds like the patient’s got marbles in their mouth,” Amin says.
The final letter stands for time to call 9-1-1, and the same holds true when it comes to TIA, even if the symptoms stop before you get to the phone.
Another symptom to pay attention to is vision change, Amin says. “The classic type of vision symptom that suggest a stroke or TIA is a blackout of vision. So if someone notices complete vision loss in just one eye, and it’s described as kind of a nightshade coming down over one eye, if it’s temporary or if it’s lasting, that is an emergency,” he says.
In fact, some stroke awareness campaigns use the acronym BE FAST, with the “B” standing for balance and the “E” representing eye/vision changes. Thinking back, Bonness says had she known about BE FAST — she had at least three of the symptoms — she “probably would have gone to the ER sooner.”
“It’s imperative that we don’t ignore those symptoms and seek medical attention very quickly,” Jivan says. “Even though they’re transient and they’re short-lived, [TIAs] are associated with long-term, worse outcomes.”
Diagnosis and treatment can help prevent a stroke
Doctors can diagnose a TIA with a series of tests in the emergency room, including imaging tests to look for signs of narrowing arteries that lead to the brain, and blood work to rule out other conditions that present with similar symptoms. After a diagnosis is established, cardiac tests may be ordered to assess heart risks that may have caused the TIA, such as atrial fibrillation, an irregular heart rhythm that can increase the risk for stroke.
The AHA also recommends that physicians assess a patient’s risk of stroke after a TIA, taking into account their age and other stroke-related risk factors, such as diabetes, high cholesterol, and high blood pressure. Those at high risk may be hospitalized. Patients at lower risk may be prescribed medications, like statins or blood thinners, or referred for surgery to open up a narrowed artery.
And because behaviors like smoking, poor nutrition, and physical inactivity can increase the likelihood of TIA or stroke, many TIA patients are counseled on risk reduction.
“We think about how to best manage those risk factors to prevent something like that from happening again,” Jivan says. Research suggests that up to 80 percent of strokes after a TIA may be preventable when risk factors are managed.
After her stroke, Bonness, now 65, poured her focus into changing her lifestyle. In addition to taking medication for high blood pressure and high cholesterol, she altered her diet, set boundaries with her work, and carved out time for creative projects, including poetry and memoir writing.
“Your lifestyle matters — so all the stuff they tell you about eating healthy and managing your stress would have helped prevent this TIA for me,” says Bonness, who fully recovered from her stroke and was eventually able to go off all of her stroke-related medications. “And it certainly has helped me prevent any future strokes now, with the lifestyle that I take very seriously.”
This article first appeared on aarp.org


